Chronic leg ulcers with heavy exudate often lead to persistent leakage, maceration, and patient discomfort. This case study shows how a superabsorbent dressing helped regain control: protecting the skin, reducing dressing changes, and easing both patient distress and nursing workload. The result – faster progress toward healing and a better quality of life.
Patient with a chronic leg ulcer and high exudate levels
Ongoing leakage causing skin breakdown and discomfort
Frequent dressing changes, consuming time and resources
Introduction of a superabsorbent dressing
Key dressing properties: high absorption, retention, and protection against leakage
Applied in routine care with immediate improvements in handling exudate
Leakage controlled, periwound skin condition improved
Reduced frequency of dressing changes
Patient comfort increased, greater freedom in daily life
Nurses reported less stress and easier wound management

The patient’s wound history presents a challenging case involving a 77-year-old man with a longstanding leg ulcer. This individual, suffering from mental illness, had been struggling with this wound for eight years without any signs of healing, as it remained stuck in the inflammation phase.
The situation was further complicated by the inability to control the vast amounts of wound exudate, which constantly leaked onto the patient’s clothes, bandages, and sheets. Consequently, the patient’s overall quality of life was severely impaired, and the healthcare provider was left feeling helpless, having exhausted all available treatment options.
This case highlights the importance of delivering effective patient care to manage chronic wounds and enhance the well-being of patients in similar situations. Studies confirmThe impact of chronic venous leg ulcers: a systematic review. J Green, R Jester, R McKinley, A Pooler. Journal of Wound Care. 2014 that challenges with leg ulcer leakage and odour can lead to social isolation, depression, low mood, and diminished self-esteem.
The symptomsSymptoms - Venous leg ulcer. 2022, NHS UK of a venous leg ulcer include pain, itching, swelling with occasional eczema and scaling in the affected leg. A venous leg ulcer often develops on the lower leg, around the ankle, where discoloured or hardened skin around the ulcer and exudate may also be present.
The inflammation phase
This process begins simultaneously with the development of the wound and is the first step in the healing process. Next, the inflammation phase means the wound is cleaned, aided by the body’s white blood cells.
The proliferation phase
The proliferation phase is when new tissue is formed. The signs of inflammation disappear, and the wound becomes bright red, looking healthier as new blood vessels grow at the surface.
The maturation phase
The final stage can last for more than a year, depending on the size and nature of the wound. During this period, the skin’s collagen is strengthened, and the bright red scar fades.

When choosing a dressing, it is essential to consider the stage of the wound healing process. Dressings should be selected based on wound location, size, exudate level, presence of infection, and surrounding skin properties.

Please provide your details and we’ll send free samples to your workplace.
Wound exudate under normal circumstances is beneficial to wound healing because it contains many components, such as biochemical modulators, growth factors and cells, which are intimately involved and beneficial to the healing process. However, in some hard-to-heal wounds, dysfunction and prolongation of normal phases can lead to further tissue damageExudate: friend or foe? Menna Lloyd Jones, British Journal of Community Nursing, 2014 around the wound area.
To enhance the wound healing process, the objectives for managing this leg ulcer were established with the aim of:

Cleaning and caringImplementing TIMERS: the race against hard-to-heal wounds. Leanne Atkin, Zofia Bućko, Elena Conde Montero, Keith Cutting, Christine Moffatt, Astrid Probst, Marco Romanelli, Gregory S Schultz, William Tettelbach. Journal of Wound Care, 2019. for the wound area is crucial in treating venous leg ulcers. A biofilm can prevent healing, and mechanical wound cleaning is recommended to remove wound debris. To remove devitalised tissue from a wound, debridement using a blade or scissors is necessary. This should only be performed by a licensed clinician qualified to practice this technique.
Pain relief is also essential during wound cleansing. An assessment of any pain the patient feels should be carried out using a validated pain scale.

In this case, our superabsorbent in DryMax Super was used as a primary dressing. These dressings can be stacked on top of each other, thus handling the worst fluid peaks that can occur when the wound is out of the inflammation phase.
Dressing changes depend on the exudate amount and wound type. Infected or highly exuding ulcers require more frequent changes. Effective dressings reduce the frequency of changes and promote healing. Superabsorbent dressings that encapsulate the exudate and keep the surface of the dressing dry are the ideal choice for use with compression therapy. Dressings with great absorptive capacity can also help prevent maceration, leakage, and odour.

Venous leg ulcers are caused by damaged venous valves in the legs, which result in impaired blood and lymph circulation. This leads to oedema, a swelling caused by fluid build-up in the lower limbs. To reduce oedema, compression therapy is recommendedSimplifying venous leg ulcer management, Consensus recommendations. Harding K, et al. Wounds International 2015..
Counteracting the oedema is the most critical aspect of treatment. Therefore, initial non-invasive imaging with venous duplex ultrasonography, arterial pulse examination, and ankle brachial pressure index measurement is recommendedNoninvasive Arterial Testing: What and When to Use for all patients with a suspected Venous leg ulcer.
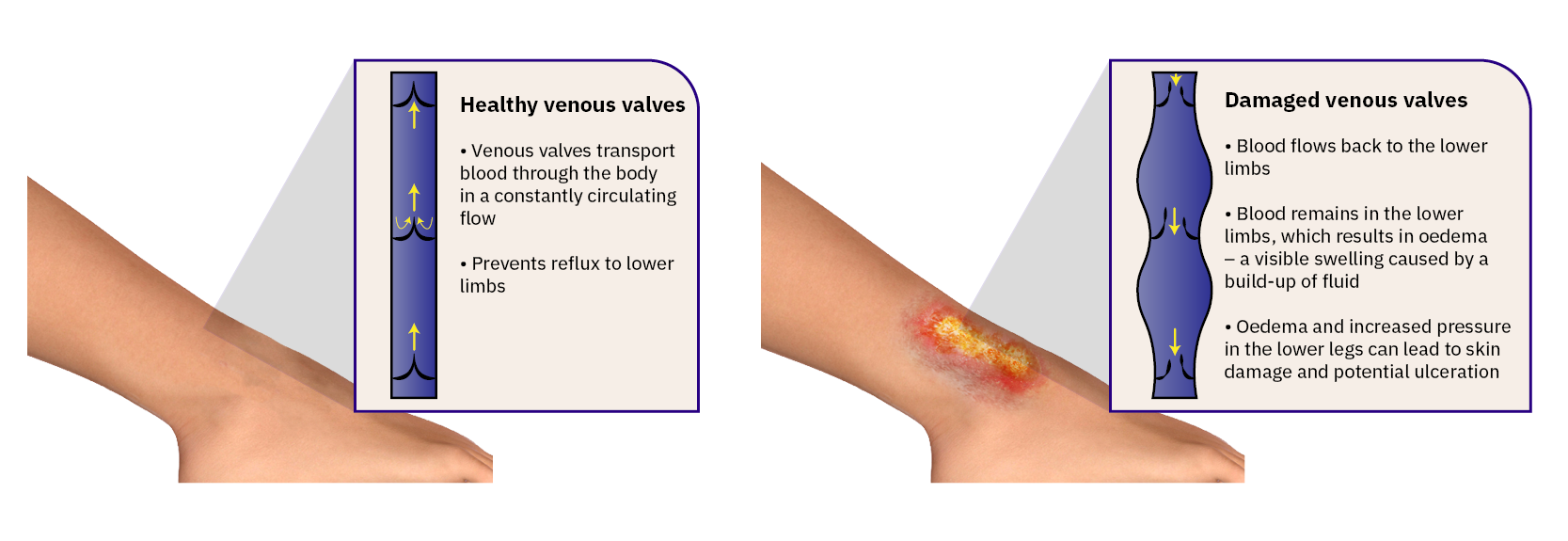
Compression therapy improves venous return, reduces swelling in the lower leg, and reduces leakage from the exuding wound. A reduction in wound exudate facilitates improved peri-wound skin condition. In addition, correct exudate management will extend dressing wear time and reduce nurse visits.

Absorbest DryMax Super dressing was used to manage the copious amounts of exudate.
![]()

Absorbest DryMax Super dressing was used. The nurse felt confident and safe using the superabsorbent dressing and didn’t want to change. Alternatively, a superabsorbent Foam dressing could have been appropriate for absorbent and protective properties.

To keep the moisture balance, a border product can be used in this stage, with ceased exudate levels.
In this case, the patient and the clinician rated the fluid handling improved with the superabsorbent dressing, achieving the primary objective of wound exudate management whilst also allowing undisturbed and preventing damage to the peri-wound skin. A result was a reduced need for clinic attendance, which freed up valuable clinic space for other patients and reduced inconvenience for the patient.

Experience the difference and compare the outcome with our superabsorbent dressing. Designed to create a simple wound healing process and optimal healing environments to support clinicians giving quality care.
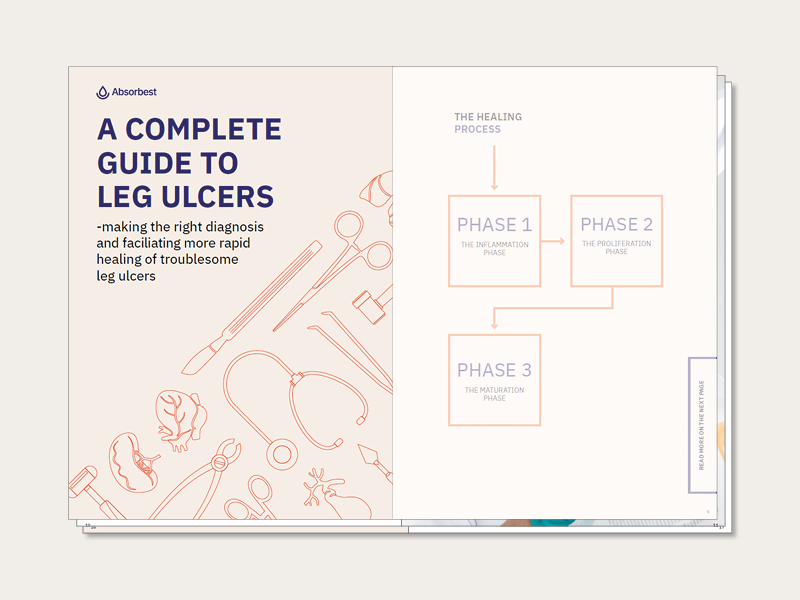
What are the characteristics of different leg ulcers, and how can we promote the healing of problematic ulcers? Treatment measures, phases of healing, cleaning, and appropriate dressings. Our complete guide to leg ulcers focuses primarily on venous ulcers, from cause and origin to the healing process and aftercare.
“The impact of chronic venous leg ulcers: a systematic review”. J Green, R Jester, R McKinley, A Pooler. Journal of Wound Care. 2014. National Library Of Medicine.
“Symptoms venous leg ulcer”. NHS UK
“Exudate: friend or foe?” Menna Lloyd Jones Br J Community Nurs. 2014. National Library of Medicine
“Implementing TIMERS: the race against hard-to-heal wounds” Leanne Atkin, Zofia Bućko, Elena Conde Montero, Keith Cutting, Christine Moffatt, Astrid Probst, Marco Romanelli, Gregory S Schultz, William Tettelbach. Journal of Wound Care, 2019.
“Noninvasive Arterial Testing: What and When to Use” Derek Mittleider, guest editors, Paul Rochon, MD and Parag J. Patel, published online 2019. National Library of Medicine.
“Simplifying venous leg ulcer management, Consensus recommendations.” Harding K, et al. Wounds International 2015. www.woundsinternational.com
“The Four Stages of Wound Healing” WoundSource Editors, 2016. WoundSource.com