Please provide your details and we will send you a download link to your e-mail.
Our “Complete Guide to leg ulcers” focuses primarily on hard-to-heal venous leg ulcers.
Learn more about treatment measures, healing phases, cleaning, and appropriate dressings, which can affect and drive the long-term healing process.
Learn more about identifying various leg ulcers
What are the underlying causes of venous leg ulcers?
Guiding: from origin to the healing process and aftercare
Please provide your details and we will send you a download link to your e-mail.
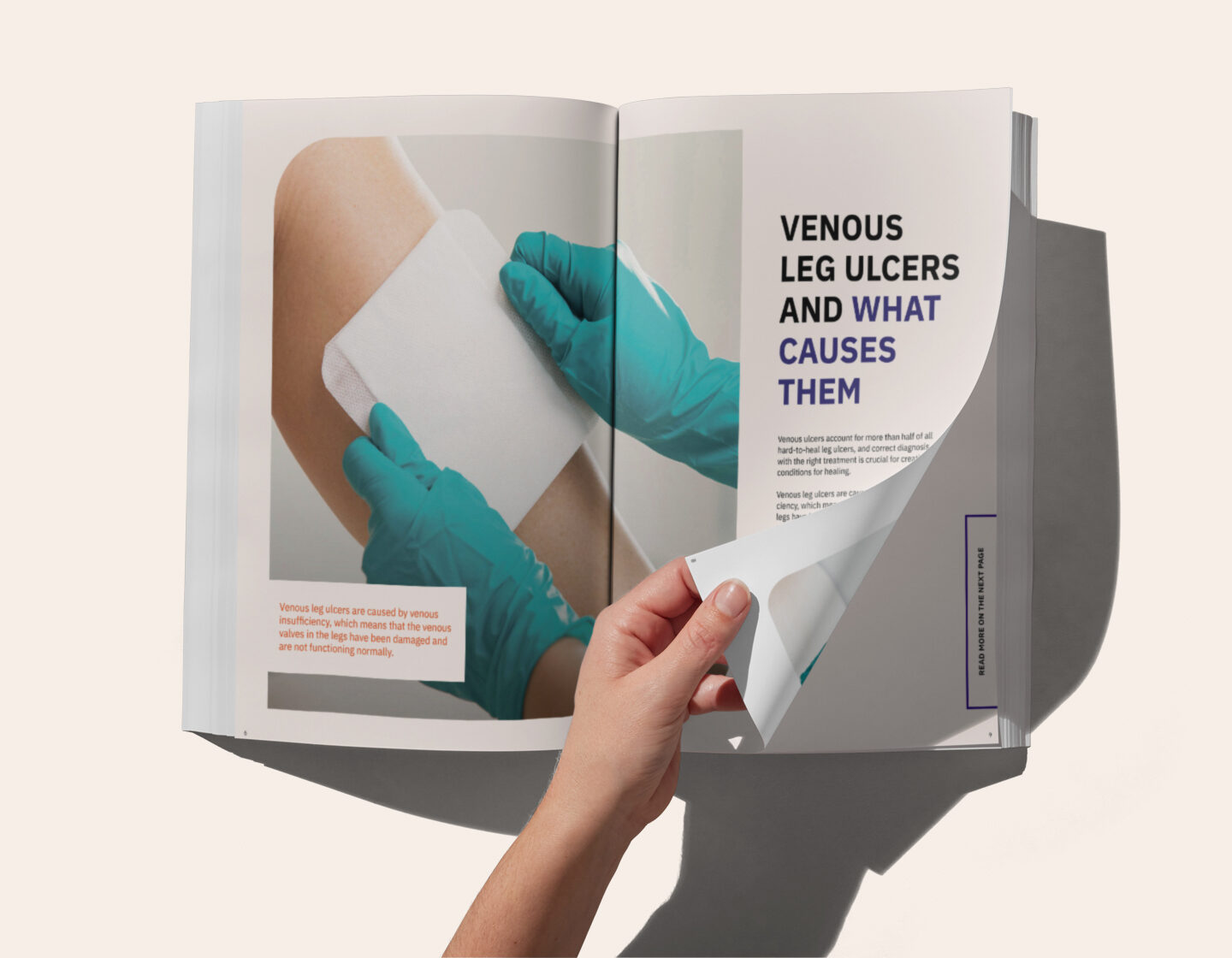
Venous leg ulcers are caused by venous insufficiency, which means that the venous valves in the legs have been damaged and are not functioning normally. The venous valves are designed to help push blood and lymph around the body in a constantly circulating flow. Dysfunctional venous valves mean that a significant portion of fluid remains in the lower limbs, which results in oedema – a visible swelling caused by a build-up of fluid.
Oedema and increased pressure in the lower legs leads to the skin being damaged from the inside and the potential for ulceration. External factors, such as a blow or impact to a lower leg with venous insufficiency, may also cause an exuding wound to develop. The fluid, known as exudate, leaks from the wound and a hard-to-heal, exuding venous ulcer forms.

Ann-Mari Fagerdahl, Associate Professor/Nurse, Wound Centre, Södersjukhuset, Sweden
This guide to leg ulcer management will help you to understand various wounds and, what distinguishes them, and how to manage them during and after the healing process.
Leg ulcers may be venous or arterial, but there are also diabetic foot ulcers, pressure ulcers or malignant leg ulcers.
Venous leg ulcers are the most common type of leg ulcer. The ulcer often develops on the inside of the lower leg, around the ankle, and a characteristic feature is the superficial ulceration. The leg is often swollen due to the venous valves not functioning normally, which often causes a heavily exuding wound. The skin around the ulcer may be discoloured, and there may be signs of eczema and scaling.
Arterial ulcers tend to occur on the foot but may also develop on the lower leg. An arterial ulcer is often deep and painful for the patient. The wound’s appearance can vary, and it will often be dry with black and yellow necrotic tissue. Ulcers are caused by interrupted arterial circulation, with surgery required to restore the circulation. Poor arterial circulation is diagnosed by recording the patient’s blood pressure at the ankle and comparing it with the pressure in the arm. If the pressure is lower at the ankle, a consultation should be arranged with a vascular surgeon.
Common causes of diabetic foot ulcers are poor peripheral circulation or peripheral nerve damage. For example, a loss of sensation in the feet and toes can lead to ulcers developing after chafing or pressure from shoes. 15% of adults with diabetes will develop a diabetic foot ulcer at some point in their life.
Pressure ulcers on the legs usually occur in vulnerable areas such as the ankle and heel. Tissue sensitivity to pressure varies, and pressure ulcers can develop under high pressure in a short time or under low pressure over a more extended period. The pressure causes a lack of oxygen locally and tissue necrosis, which leads to ulceration. In the case of a pressure ulcer, relieving the pressure is an essential aspect of wound care. Prevention measures (pressure ulcer prophylaxis) are vital to prevent pressure ulcers.
Malignant leg ulcers may be considered a type of fungating wound and a wound resulting from tissue in another type of leg ulcer having undergone a malignant transformation.
Venous leg ulcers are typically caused by venous insufficiency, which means the venous valves in the legs have been damaged and are not functioning normally. The venous valves are designed to help push blood and lymph around the body in a constantly circulating flow. Dysfunctional venous valves mean that a significant portion of
fluid remains in the lower limbs, which results in oedema – a visible swelling caused by a build-up of fluid.
The inflammation phase starts simultaneously as the wound develops and is the first step in the healing process. The inflammation phase means that the wound is being cleaned, a process that
is aided by the body’s white blood cells.
The proliferation phase is when new tissue is formed. The signs of inflammation disappear, the wound becomes bright red and looks healthier as new blood vessels grow at the surface. Small bumps may be formed by the tiny growths that gradually fill the wound. Cells that secrete collagen develop and create new tissue; the wound area shrinks as the wound contracts. During the proliferation phase, growth may continue beyond what is needed to fill the wound. This leads to what is called hypergranulation, which is not part of the normal healing process.
The final stage of wound healing is the maturation phase. This can last for more than a year, depending on the size and nature of the wound. During this period, the skin’s collagen is strengthened, and the bright red scar fades over time.
Compression is the mainstay of treatment in wounds caused by venous insufficiency; a compression
bandage can sometimes be left untouched for a week. For this reason, a suitable wound dressing is crucial; for example, a superabsorbent dressing with a dressing change frequency matching that of the compression therapy, not the other way around.
The compression bandage is a vital treatment measure in cases of a venous leg ulcer. When the leg is bandaged for compression, it makes it easier for venous blood and lymph to leave the leg and be transported back to the heart.
Compression therapy reduces swelling in the lower leg, and there is reduced leakage from the exuding wound. Less exudate makes for an improved wound edge environment, and the interval between treatments can be extended.
There are currently several compression systems to choose from. Short–, medium– or long-stretch bandages are used depending on the patient’s level of mobility. The manufacturer’s instructions
explain how the bandage is to be applied.
The guide “Simplifying venous leg ulcer management” provides clear guidelines for compression therapy. The guide is, therefore, a good support tool when choosing a compression system with the correct compression dose based on the patient’s diagnosis.