The aim of managing and dressing a venous leg ulcer is to create optimum conditions for healing. Ensuring a good wound environment and managing oedema positively impact the wound-healing process. This is done by cleaning the wound thoroughly and using appropriate dressings and compression therapy. Understanding the patient’s history and any present comorbidity factors is vital for treatment and understanding why the patient has an exuding wound. A hard-to-heal leg ulcer is, in itself, indicative of an underlying cause.

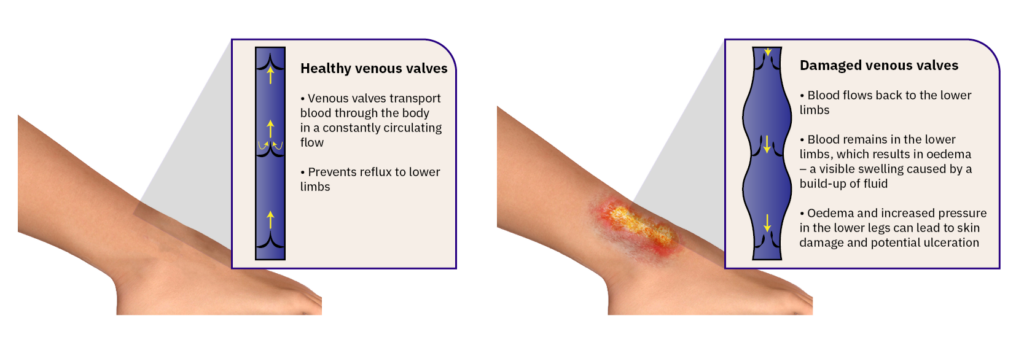
Venous leg ulcers are caused by venous insufficiency, which means the venous valves in the legs have been damaged and are not functioning normally. The venous valves are designed to help push blood and lymph around the body in a constantly circulating flow. Dysfunctional venous valves mean that a significant portion of fluid remains in the lower limbs, resulting in oedema – a swelling caused by fluid build-up. An international group of experts has recommendedSimplifying venous leg ulcer management: consensus recommendations. woundsinternational.com using compression therapy as far as possible to reduce the oedema.
Counteracting the oedema is the most critical aspect of managing leg ulcers.
Compression therapy improves venous return, reduces swelling in the lower leg, and reduces leakage from the exuding wound. Reducing wound exudate facilitates improved peri-wound skin condition. In addition, correct exudate management will extend dressing wear time and minimise nurse visits. There are currently several compression systems to choose from. Compression management includes long—and short-stretch bandage systems and kits. The manufacturer’s instructions explain how the bandage is to be applied.
![]()
Some solutions use adjustable compression in addition to bandages. These form compression stockings with a Velcro wrap system that is adjusted to produce the required degree of compression. An inflatable boot may prove a valuable complement to other compression methods. With a holistic assessment, monitoring the reduction in oedema provides insight into the effectiveness of treating venous leg ulcers.
Wound exudate, often called “wound fluid” or “wound drainage”, is vital to wound healing. It consists of fluid that leaks out of blood vessels and closely resembles blood plasma“A clinical observational case series evaluation of a superabsorbent dressing on exudating wounds“, British Journal of Nursing, 2024, Vol 33.. Exudate helps maintain a moist environment, carries nutrients and tissue-repairing cells, and facilitates the natural removal of dead tissue (autolytic debridement).
However, exudate can also hinder healing if it is excessive, located in the wrong area, or has an inappropriate composition, particularly in chronic wounds. The primary role of exudate is to support the diffusion of healing factors and the migration of cells across the wound bed, which are essential for the wound healing process.
Ensuring the right balance of exudate is crucial, as both too much or too little can significantly delay healing“Wound exudate and the role of dressings. A consensus document“, Int. Wound J. 2008. Effective wound management aims to maintain this balance, promoting a moist environment that enhances healing rates, reduces discomfort, and minimises the risk of infection. This balance is vital in managing chronic, hard-to-heal wounds where exudate can be excessive due to prolonged inflammation.
Heavily exuding wounds can cause problems and be distressing for the patient. Exudate is a natural and vital part of a healthy wound-healing process. Exudate keeps the wound moist and contains nutrients, proteins, and growth factors that promote healing and help form new tissue. The objective is to create optimal moisture conditions—a healthy environment for the peri-wound skin to ensure it continues acting as a protective barrier.
The exudate in hard-to-heal wounds contains increased levels of inflammatory molecules, which keep the wound in the inflammation phase and can cause more exudate to be produced. This can lead to an infection, resulting in pain, discomfort, and a reduction in the patient’s quality of life, potentially delaying the wound healing process.
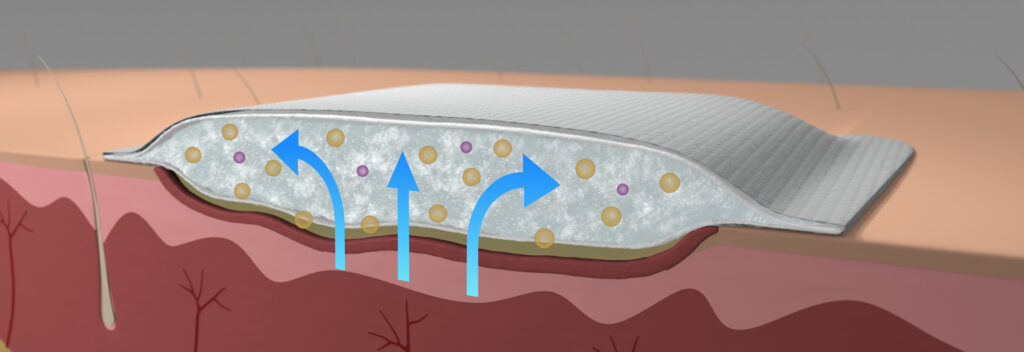
It is essential to remove excess exudate that may be present. Superabsorbent dressings are advised as they can lock the exudate within the dressing. This provides optimal moisture conditions and a healthy environment for the peri-wound skin.
When assessing and treating hard-to-heal venous leg ulcers, it is necessary to monitor the size and appearance of the wound area. Examining the wound’s edges and measuring its size indicates if healing is progressing. If the patient has an ulcer that produces excessive exudate, its edges and skin may be macerated. Clinical documentation is taken to record the wound and peri-wound skin progress. The wound edges can, for example, be described as rolling, punched-out, macerated or epithelialised. The nature of the wound area must be carefully explained to determine whether the wound has a fibrin coating, is granulating or is necrotic. It may also be helpful to photograph the ulcer for documentation purposes.
![]()
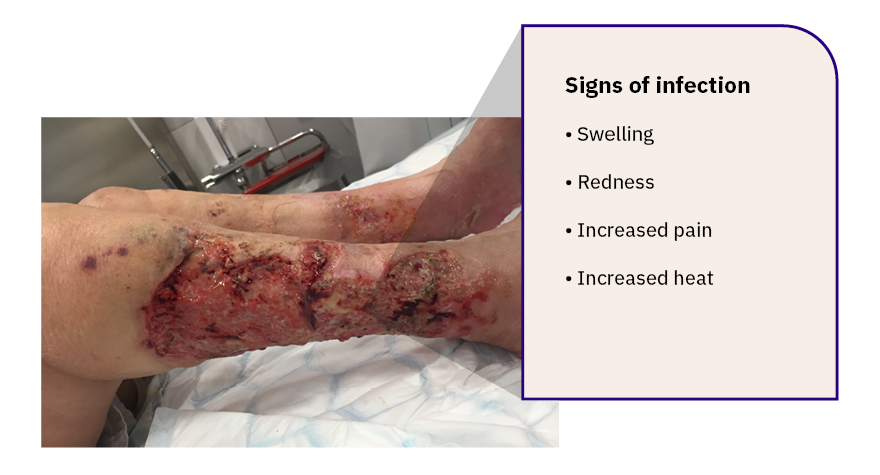
Delayed wound healing usually occurs in the proliferation phase. Long-standing wounds have an increased risk of infection, enabling bacteria to proliferate. The bacteria thrive in moist conditions, and the more exudate and moisture in the wound, the more bacteria there will be. Bacteria are always present on the surface of a wound. Usually, these are bacteria from the skin and mucosal flora, such as staphylococci, enterococci and intestinal bacteria, but other bacteria may also be present. An infection can develop if the bacteria penetrate the wound deeper and multiply.
The patient will often experience the clinical signs of infection, i.e., an increase in pain, swelling, redness, and exudate, and the patient may also experience general malaise. However, it is worth remembering that people with diabetes can have reduced sensation and not exhibit pain (known as neuropathy). Redness, increased discharge from the wound, odour and swelling are other indications that a leg ulcer has become infected. Where infection is suspected, a clinical assessment must be performed to assess the need for antimicrobial wound dressings, antibiotic therapy, or wound swabs for culture and sensitivity testing.
Cleaning the wound thoroughly when changing dressings is important to remove wound debris. Saline solution or tap water may be used to clean a wound. Local guidelines for wound cleansing techniques, including antimicrobial wash lotions, may also be advised. The wound usually has debris, e.g., fibrin and dried exudate. Such deposits can be removed through mechanical wound cleaning, such as using a gentle monofilament pad. Removing devitalised tissue and wound debris is vital for wound healing progress. Several debridement techniques can achieve this, including surgical, biological enzymatic, mechanical, and autolytic debridement. Debridement is a specialised technique and should always be performed by a licensed clinician qualified to practice this technique.
![]()
In conjunction with wound cleansing, debridement, and chosen dressing, it is also necessary to consider suitable pain relief. A holistic assessment, including management of any pain the patient is experiencing via a validated pain scale, should also be noted. Before treating venous leg ulcers, an assessment of any pain the patient experiences should be done using a validated pain scale. Based on clinical assessment, a qualified clinician may require and prescribe analgesia. Pain medication may be administered orally or by injection or be applied topically to the wound as a gel, spray or ointment. If using a spray, for example, this will take effect within 1-5 minutes.
Please provide your details and we will send you a download link to your e-mail.
Dressing changes depend on several factors, including the amount of exudate present. Ulcers that produce excessive exudate or are infected require dressings to be changed more frequently. The nature of the wound also impacts the type of wound care products that will best promote healing and a successful long-term outcome.
A dressing that can manage exudate and facilitate wound healing leads to a reduced frequency of dressing changes. Dressing choice and absorption ability should ideally correspond with the treatment regime where compression therapy is part of the patient’s treatment plan.
A superabsorbent dressing is designed to work best with exuding wounds because the dressing absorbs and encapsulates the exudate, forming a gel inside the dressing’s core. Superabsorbent dressings that facilitates extended wear time benefits both patient and healthcare services. The dressing has properties that promote more rapid healing, which spares the patient uncertainty, time and pain. The dressing’s excellent absorptive capacity means fewer dressing changes, as the surface of the dressing remains dry. Dressings should reduce the risk of the peri-wound skin becoming macerated.
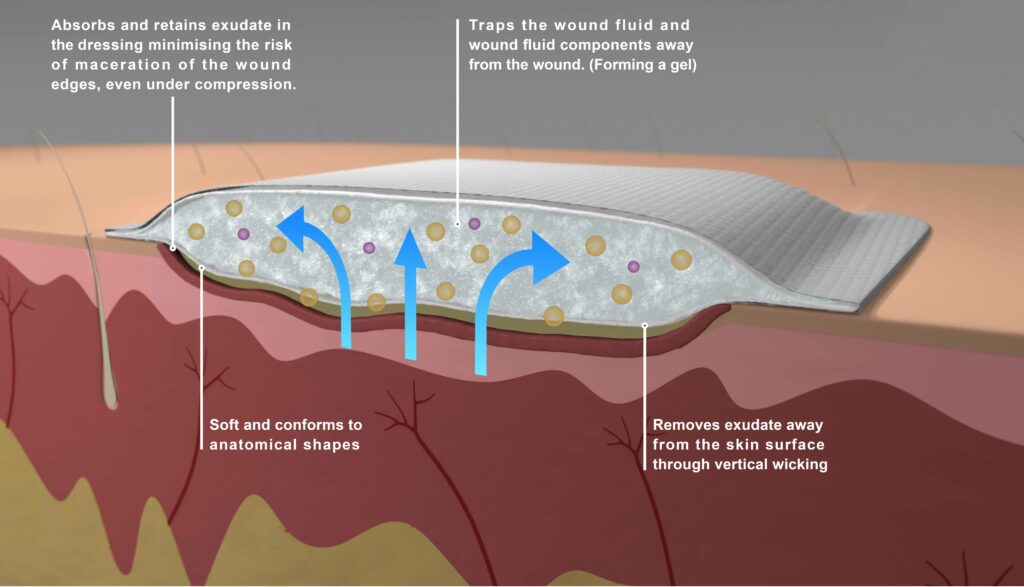
Superabsorbent dressings that encapsulate the exudate and keep the surface of the dressing dry are the ideal choice for use with compression therapy. The dressings come in various formats and sizes and all have great absorptive capacity. This makes it easy for the caregiver to choose a dressing suitable for a particular type and size of wound.
Dressing a wound is just one treatment measure in the lengthy process of treating a hard-to-heal ulcer, which can require lifelong follow-up care. If managed inappropriately, ulcers tend to reoccur. And can be resource dependent and problematic for the patient. Here you will find more information about how best to treat a venous leg ulcer to reduce the impact of hard-to-heal wounds.
Experience the difference and compare the outcome with our superabsorbent dressing. Designed to create a simple wound healing process and optimal healing environments to support clinicians giving quality care.
A premium dressing made in Sweden.
This complete guide to leg ulcers will help you to understand various wounds, what distinguishes these, and how they can best be treated during and after the healing process.
Harding, K., et al. Simplifying venous leg ulcer management, Consensus recommendations. Wounds International, 2015, Available to download from www.woundsinternational.com
Mark Collier “A clinical observational case series evaluation of a superabsorbent dressing on exudating wounds“, British Journal of Nursing, 2024, Vol 33.
Expert Working group “Wound exudate and the role of dressings. A consensus document“, Int. Wound J. 2008. National Library of Medicine.
Höglin G, Freijd H. A cohort study to investigate the benefit of the use of DryMax Extra superabsorbent wound dressing on a population of wet wounds, 2011; Poster presentation, Harrogate.
Lindholm C. MD, professor, Sophiahemmet University, Stockholm, 2018, www.vardhandboken.se
Lindholm C. Sår. Uppl 4:2 Studentlitteratur AB, 2018