This study aimed to evaluate the performance of a superabsorbent dressing* on patients with exuding burn wounds.
Eight patients, aged 28-77 years, participated in this open case study. The patients were recruited and selected from a Swedish University hospital burn centre over a period of 20 months because of their exuding wounds, ranging from superficial dermal to full-thickness burns.
Standard protocols were applied to patients included in the study. The standard procedure for this type of injury is to cover the wound with silver sulfadiazine cream to prevent infection, followed by a non-adherent wound contact layer covered by fluffy gauze and secured with roller and/or tubular bandages. During the study period, fluffy gauze was replaced with the superabsorbent dressing*.
Most patients were anaesthetized or sedated, at least during cleaning and dressing changes. The time of participation in the study ranged between two and 12 days, with an average length of seven days.
In all eight cases, the clinicians found the superabsorbent wound dressing* superior to standard treatment, i.e. fluffy gauze, in its ability to manage exudate and prevent maceration and hypothermia. The dressing* absorbed not only thin but thick wound fluid efficiently, compared to other dressings, and also absorbed blood into the dressing*, although the red blood cells were trapped on the dressing surface. Furthermore, the dressing* was easy to use, and the big sizes could cover large wound areas. The clinicians would recommend the superabsorbent wound dressing* for their local wound treatment program in seven out of eight cases.
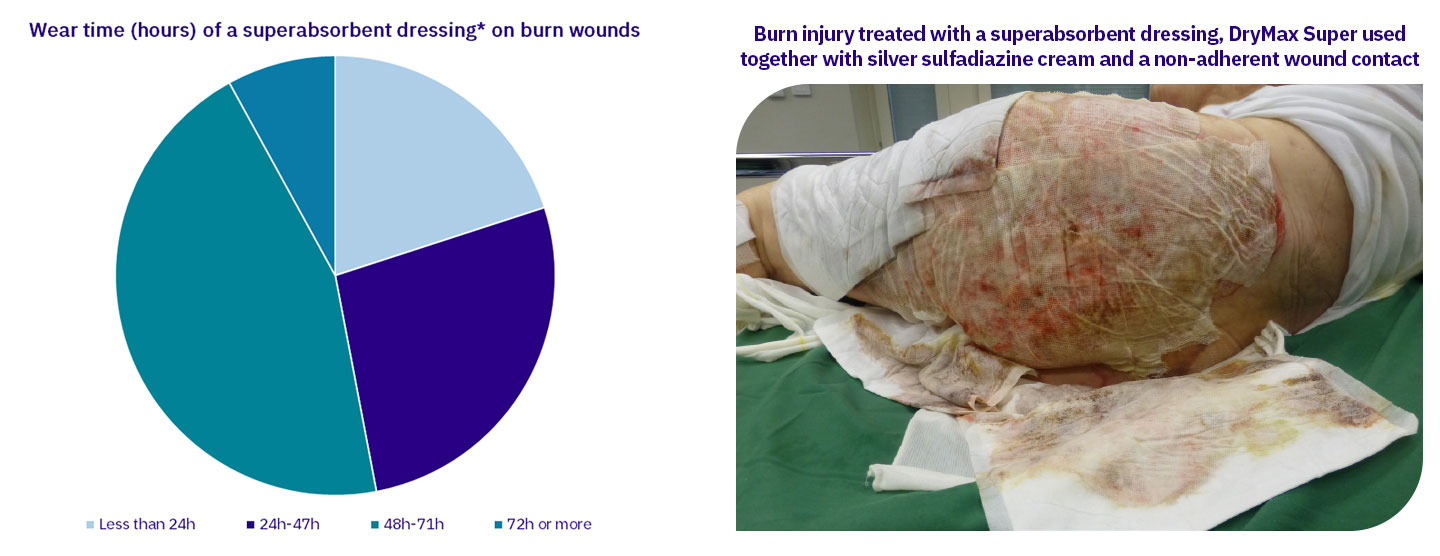
In this study, dressing changes were generally performed because of routine procedures and the need for wound inspection, not because of leakage. Most dressings were used for more than 48 hours on the wounds.

A forty-four-year-old man with circumferential fire burns on both thighs. The injuries were 2.5% deep dermal and 2.5% full-thickness burns.
Twelve hours after the injury, the wounds were treated for 12 days with standard procedure, but the fluffy gauze was replaced with a superabsorbent dressing*. During this time, the wounds were cleaned, and the dressings* were changed on six occasions while the patient was anaesthetized or sedated. The patient and the bed remained dry; there was no maceration to the surrounding skin and no decrease in skin temperature.
In connection with each dressing* change, the removed superabsorbent dressings from each thigh were weighed and reached their highest weight on day 4. The superabsorbent dressing* did not stick to the wounds. On the 12th day, the patient had an operation and skin transplants.
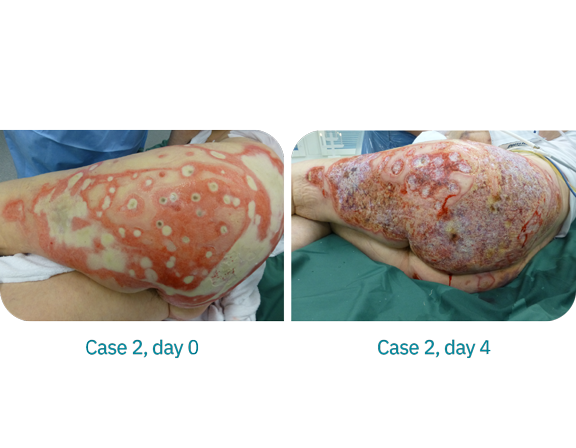
A seventy-seven-year-old woman with contact burns on the left hip, buttock, and leg. The injuries were 1.5% superficial dermal, 2.5% deep dermal, and 3% full-thickness burns.
Twenty-four hours after the injury, the wounds were treated for seven days with standard procedure. Still, the silver sulfadiazine cream was omitted, and the fluffy gauze was replaced with the superabsorbent dressing*. Due to the use of bromelain-based debridement, the wounds were cleaned, and the dressings* changed daily even though they were not completely saturated.
The patient had continuous pain relief with paracetamol and oxycodone/naloxone and was also premedicated or sedated before wound cleaning and dressing* changes. On three occasions, the reports mention slight or moderate pain when the dressings* were removed, but no pain was reported during wear time. The patient and the bed remained dry, and there was no maceration to the surrounding skin, except on day 4, when there was slight maceration to the wound edges of the upper part of the hip where there had been more exudation. There was no decrease in skin temperature.
The superabsorbent dressing* did not stick to the wounds. In connection with each dressing* change, the removed superabsorbent dressings* were weighed and reached their highest weight on day 3.
This study aims to evaluate the performance of the superabsorbent dressing* on patients with exuding burn wounds. The results from the study indicate that the evaluated superabsorbent dressing* meets the requirements for an ideal burn wound dressing4,5 in terms of its absorption and retention capacity of both thick and thin wound fluid and, unlike most other dressings, also blood, properties which have been demonstrated in other studies9,10,11.
It has been verified that leaving dressed wounds undisturbed using wound dressings that allow longer wear time helps healing6,7. In this study, the superabsorbent dressing* was only left in place once fully saturated but was removed based on the routine procedure and the need for wound inspection. Consequently, the efficiency and cost-effectiveness of the superabsorbent dressing* on patients with exuding burn wounds cannot be fully evaluated. Other limitations of this study include the need for uniformity regarding data reporting, despite standard protocols, and the absence of records on the use of antibiotics.
Further studies focusing on wound dressings’ ability to control infection are needed. It would be interesting to study the frequency of wound infection in burn injuries treated with traditional wound dressings compared to superabsorbent dressings, as well as the frequency of wound infections in burn injuries where wound dressings are changed according to the routine procedure compared to superabsorbent dressings that are left in place until fully saturated.
Results from this case series indicate that the evaluated superabsorbent dressing* is a suitable choice for exuding burn wounds because of its excellent capacity to manage various types of wound exudate and prevent leakage, maceration, and hypothermia, thus supporting patient recovery. Larger-scale clinical studies will be necessary to confirm these findings and provide more data for further analysis.

Experience the difference and compare the outcome with our superabsorbent dressing. Designed to create a simple wound healing process and optimal healing environments to support clinicians giving quality care.
A premium dressing made in Sweden.