Every year, the Wound Care Symposium in Sweden brings together healthcare professionals, speakers, and industry experts for two days of shared learning and inspiration, focusing on “hard-to-heal wounds.”
The event highlights innovation, best practice and practical insights, combining lectures with valuable networking among exhibitors presenting the latest in wound care.
One of the speakers in 2022 was Susanne Dufva, oncology nurse specialist at the Wound Centre, Södersjukhuset, Stockholm, and Chair of the Swedish Wound Nurses Association (SSiS).
After her session on “The Wound Healing Process and Dressings,” we had the opportunity to discuss how clinical knowledge and daily practice converge when selecting the appropriate dressing.*
Susanne’s extensive experience is evident. She speaks candidly and clearly about wound care, emphasising, above all, the importance of an established diagnosis before focusing on dressing types. She stresses that there is no single dressing that suits all wounds; instead, the key is to choose the appropriate kind of dressing based on the phase of the wound-healing process.
“The type of dressing we use matters. We should choose products based on the wound’s appearance and align them with the healing process and its different phases: the hemostasis phase, inflammatory phase, proliferation phase, and maturation phase. We mustn’t use the same product throughout the entire healing journey.”
Several key factors should be considered when selecting a dressing. Susanne explains that the amount of wound exudate determines which type of wound dressing is appropriate.

“During the early phases, the hemostasis and inflammatory phases, it’s entirely natural for the wound to produce a lot of exudate as it cleanses itself; at the same time, it needs to be managed well. That’s when we need to use a superabsorbent dressing.”
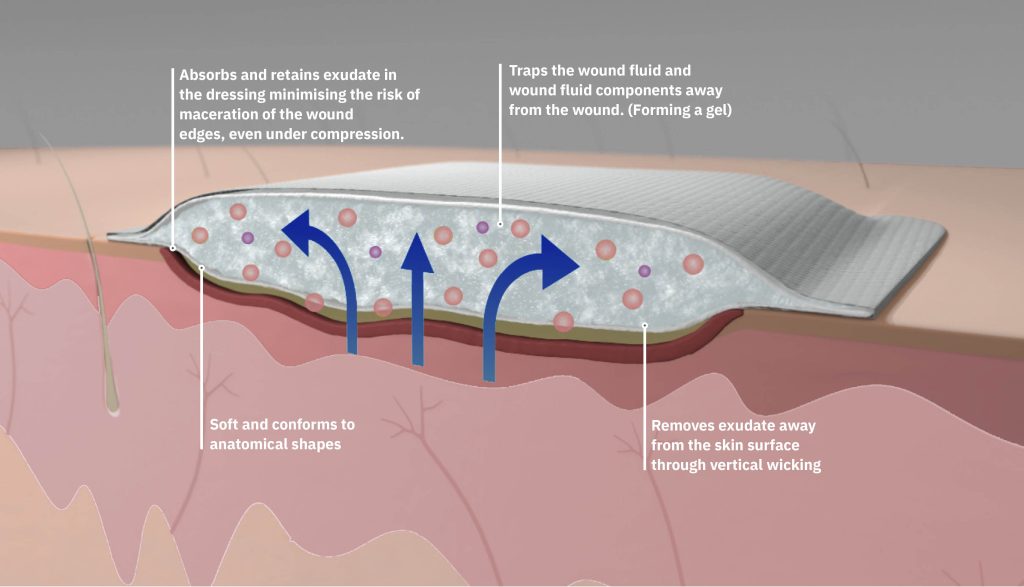
Superabsorbent dressings are designed to handle large volumes of fluid. A high-quality superabsorbent can retain fluid within the wound dressing, preventing it from remaining in contact with the patient’s skin, making it an excellent choice during the early, cleansing inflammatory phase.
Once the wound is clean, exudate levels decrease, and granulation tissue (new skin cells) begins to form, moving the wound into the proliferation phase.
“At this stage, we should use a product that protects the fragile new tissue and doesn’t interfere with the healing process. You shouldn’t need to change the dressing too frequently, and there are many excellent polyurethane foam dressings available for this phase,” says Susanne.

Even after a wound appears healed, it’s vital to continue protecting it. The wound remains in the maturation phase for an extended period.
“It can take 1–2 years for a wound to reach full strength and optimal healing. Yes, it really takes that long. Early on, it’s essential to protect the newly healed skin to avoid accidentally damaging it when, for example, the patient puts on or removes clothing,” Susanne continues.
As a nurse, being observant of the wound’s needs and wound healing phase provides direction in selecting the most suitable dressing, whether that’s to manage exudate, support an optimal healing environment, or protect the wound.
Susanne also addressed economic considerations during her talk. Both staffing costs and procurement expenses could be reduced in trusts through increased knowledge of dressings and wound management.
“We often fixate on the unit price of products and dressings. As a result, many facilities decide not to purchase the more expensive options, since the purchase costs seem too high. But this often leads to more frequent dressing changes, because we’re using products that aren’t suited to the patient’s wound”, Susanne explains.
She continues:
“This means patients may need to visit the clinic much more often, or healthcare staff must go to the patient’s home. If we don’t use high-quality dressings, this happens unnecessarily often. The products may be cheap, but they’re not good for the patient.”
![]()
Susanne emphasises that dressings selected based on the patient’s diagnosis and the wound’s healing phase can save both time and resources. In contrast, an unsuitable dressing may actually prolong the healing period.
“In some cases, the wound may never heal, or it takes far longer than necessary. But most importantly, the patient’s quality of life suffers. No patient should have to endure that unnecessarily.”
She also discusses the current reimbursement model for wound care:
“Today, [in Sweden] we receive reimbursement regardless of whether the patient visits us or we visit them. We’re compensated each time we perform wound care, but there’s no financial incentive for actually achieving wound healing.”
Finally, Susanne emphasises the importance of person-centred care, where the patient is at the centre.
She notes that healthcare professionals are often quick to offer the best solution, advice, and information—but may forget first to let the patient speak.

“Patients often have a different perspective. They know themselves best, and that’s why I believe it’s essential to start with an open-ended question, allowing the patient to explain their situation. Often, you don’t need to ask many more questions. Their story gives us a great starting point to understand how we can truly help the person in front of us.”
Susanne concludes:
“Listen. Two ears, one mouth. It’s good to listen twice as much as you speak,” she says with a smile.
![]()
*This interview was conducted in Swedish by Absorbest’s marketing manager, Jenny Rönningen and has been freely translated into English.

Discover the dressing that can help you do both. Designed to create a simple wound healing process and optimal healing environments to support clinicians in giving quality care.