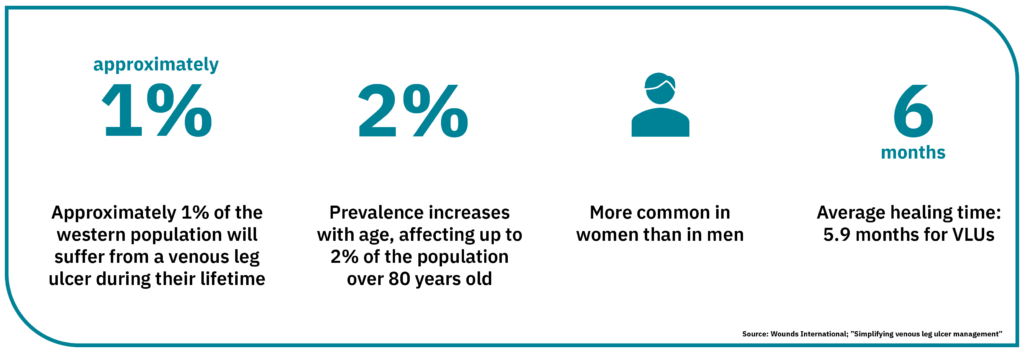
Several essential aspects must be considered for treatment of venous leg ulcers, a form of ulcer that accountsWhy Venous Leg Ulcers Have Difficulty Healing: Overview on Pathophysiology, Clinical Consequences, and Treatment. National Library Of Medicine for more than half of all hard-to-heal wounds. Compression therapy is viewed as the gold standard and evidence-based in treating leg ulcers. Correct diagnosis and, therefore, the proper treatment is crucial for creating the right conditions for healing. Patient referral may be required to other members of the multidisciplinary team.
In addition to achieving a good healing outcome, the underlying cause of the ulcer needs to be investigated and a holistic patient assessment performed. This being the case, the patient ought to be receptive to potential lifestyle changes to reduce the risk of recurrent ulcers.
The symptoms of a venous leg ulcer include pain, itching, swelling, with occasional eczema and scaling in the affected leg. A venous leg ulcer often develops on the lower leg, around the ankle, where discoloured or hardened skin around the ulcer and exudate may also be present. Therefore, initial non-invasive imaging with venous duplex ultrasonography, arterial pulse examination, and measurement of ankle brachial pressure index is recommended for all patients with a suspected Venous leg ulcer. Color duplex ultrasonographyDuplex ultrasound involves using high-frequency sound waves to look at the speed of blood flow and structure of the leg veins. The B-mode transducer (like a microphone) obtains an image of the vessel being studied. The Doppler probe within the transducer evaluates the velocity and direction of blood flow in the vessel. is also recommended to assess for deep and superficial venous reflux and obstruction.
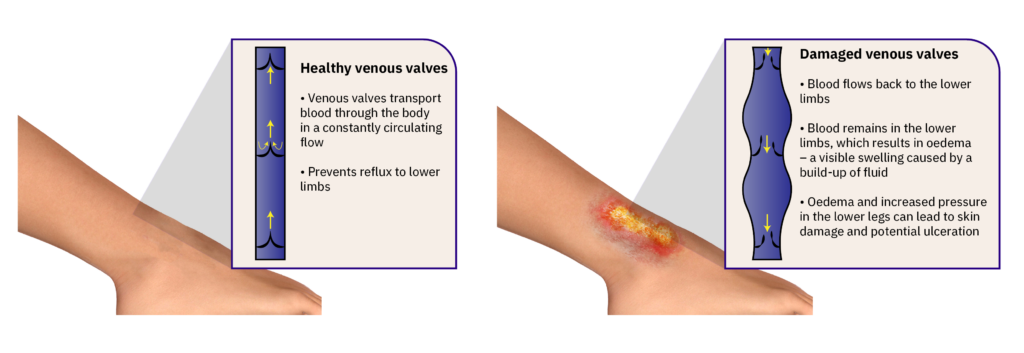
The most common underlying cause of a venous leg ulcer is venous insufficiency, which develops due to circulatory problems caused by damaged venous valves and not functioning normally. The venous valves are designed to help push blood and lymph around the body in a constantly circulating flow. Dysfunctional venous valves mean that a significant portion of fluid remains in the lower limbs, resulting in oedema – a visible swelling caused by fluid build-up. Oedema and increased pressure in the lower legs lead to the skin being damaged from the inside and the potential for ulceration. External factors, such as a blow or impact to the lower leg with venous insufficiency, may also cause an exuding wound to develop. The fluid, known as exudate, leaks from the wound and a hard-to-heal, exuding venous ulcer forms.
It takes time for a venous leg ulcer to heal, and sometimes several months of treatment are required. In general, wounds follow a healing process comprising three phases. These can also be a reference framework for the treatment measures used in hard-to-heal venous leg ulcers. The phases are defined as follows:
This starts simultaneously as the wound develops and is the first step in the healing process. Next, the inflammation phase means the wound is cleaned, aided by the body’s white blood cells.
The proliferation phase is when new tissue is formed. The signs of inflammation disappear, and the wound becomes bright red and looks healthier as new blood vessels grow at the surface. Small bumps may be formed by the tiny growths that gradually fill the wound. Cells that secrete collagen develop and form new tissue; the wound area shrinks as the wound contracts. During the proliferation phase, growth may continue beyond what is needed to fill the wound. This leads to hypergranulation, not part of the normal healing process.
The final stage of wound healing is the maturation phase. This can last for more than a year, depending on the size and nature of the wound. During this period, the skin’s collagen is strengthened, and the bright red scar fades over time.


Please provide your details and we’ll send free samples to your workplace.
In a consensus document, an international group of experts has emphasisedSimplifying venous leg ulcer management: consensus recommendations. woundsinternational.com the importance of compression therapy as a long-term treatment measure that can also reduce the risk of recurrent ulcers, which, unfortunately, is a relatively common occurrence.
Compression therapy improves venous return. Compression therapy reduces swelling in the lower leg, and there is reduced leakage from the exuding wound. A reduction in wound exudate facilitates improved peri-wound skin condition. Correct exudate management will extend dressing wear time and minimise nurse visits. There are currently several compression systems to choose from. Compression management includes long and short-stretch bandage systems and kits. The manufacturer’s instructions explain how the bandage is to be applied.
The guide ‘Simplifying venous leg ulcer management’ provides clear guidelines for compression therapy. The focus is, therefore, a good support tool when choosing a compression system with the correct compression dose based on the patient’s diagnosis. As well as compression using bandages, some solutions use adjustable compression. These form compression stockings with a Velcro wrap system, which is adjusted to produce the required degree of compression. An inflatable boot may prove a valuable complement to other compression methods.
![]()
As compression is the mainstay of treatment in cases of exuding wounds caused by venous insufficiency, a compression bandage can sometimes be left untouched for a week. For this reason, a suitable wound dressing is crucial; for example, a superabsorbent dressing with a dressing change frequency matching that of the compression therapy. In addition, it is essential to monitor the effect of compression therapy during treatment. A complete holistic assessment measuring ankle circumference indicates progress and whether the leg may need to be re-bandaged due to reduced circumference as the swelling subsides. Signs of a positive healing trajectory also help motivate the patient during treatment.
A crucial aspect of treatment in cases of venous leg ulcers is cleansing and caring for the wound area. Bacteria are always present in the wound area, but the formation of a biofilm can prevent healing. It is common for wound debris to be present in the wound, e.g., fibrin and dried exudate. For example, such deposits can be removed through mechanical wound cleansing using a soft monofilament pad. As wound cleansing can be painful, providing pain relief is vital.
Before treating arterial leg ulcers, an assessment of any pain, the patient feels should be carried out using a validated pain scale. Based on clinical assessment, a qualified clinician may require and prescribe analgesia. Pain medication may be administered orally, by injection, or be applied topically to the wound as a gel, spray, or ointment. If using a spray, for example, this will take effect within 1-5 minutes.
![]()
A clinician should consider further investigations, e.g. wound swab as per local guidelines or the commencement of antibiotic therapy, If a wound shows signs of infection, such as further swelling, redness, increased pain and heat.
If there is devitalised tissue in the wound, this often needs to be removed through debridement, which is the removal of devitalised tissue using a blade or scissors. Debridement is a specialised technique and should always be performed by a licensed clinician qualified to practice this technique.
Slight discolouration around the ankle and lower leg is a very early sign of skin changes and vericose eczema. On lighter skin, it looks red or brown. On darker skin, it looks dark brown, purple or grey and can be more challenging. If varicose eczema is not treated, leg ulcers can develop. Treatment options should be considered in consultation and dialogue with GPs.
Venous leg ulcers should heal with the correct treatment, but there is a considerable risk of recurrent venous ulcers. This is because the veins in the leg are still damaged and have not recovered their normal function. Even after the ulcer has healed, treatment must continue with medical compression hosiery for lifelong follow-up care. Other chronic conditions must also be treated. It is strongly recommended that the patient review their diet and exercise and, if a smoker, quit smoking to ensure the best conditions for treating their venous leg ulcer.

Experience the difference and compare the results with our superabsorbent dressing. Designed to simplify wound management, promote the wound healing process and create optimal healing environments that support clinicians in providing quality care.
“Why Venous Leg Ulcers Have Difficulty Healing: Overview on Pathophysiology, Clinical Consequences, and Treatment”. National Library Of Medicine.
NHS, UK Overview venous leg ulcer
Definition Duplex Ultrasound, Stanford Medicine
Harding K, et al. Simplifying venous leg ulcer management, Consensus recommendations. Wounds International 2015. www.woundsinternational.com
Vårdhandboken, Christina Lindholm, med.dr, professor, Sophiahemmet Högskola, Stockholm. www.vardhandboken.se
Lindholm C. Sår. [Wounds] Uppl 4:2 Studentlitteratur AB, 2018